How scientists in South Africa and throughout the continent plan to make use of mRNA expertise to combat ailments and sort out inequities in international well being.

Cape City, South Africa – It was early December 2021 and infections from a brand new coronavirus variant, Omicron, have been ripping by South Africa, the place 90,000 folks had already died from the pandemic.
COVID-19 circumstances had surged 255 % in a single week amongst a inhabitants wherein solely 24 % was absolutely vaccinated and the nation had hit a excessive of practically 27,000 new infections every day.
On a windy Monday morning, Dr Caryn Fenner drove the half-hour from her gated neighborhood to her office, situated in an outer industrial suburb of Cape City. Her pale blue Fiat 500 was the one car driving alongside motorways lined with powerlines and two-storey warehouses, every the scale of a soccer subject, housing espresso producers, freight corporations and steelmakers.
Fenner, who's the chief director at Afrigen Biologics & Vaccines, was racing to satisfy a decent deadline for a domestically produced mRNA vaccine. Her facility, tucked between different warehouses promoting water filtration techniques and spare bike elements, seemed unremarkable. But revolutionary work was being undertaken inside its boxy scientific rooms. Afrigen was utilizing publicly out there data to make its personal trial model of Moderna’s COVID vaccine.
When, on November 26, 2021, the World Well being Group (WHO) named Omicron a variant of concern, inside hours overseas governments imposed journey bans on half a dozen African international locations, together with South Africa.
The financial impression was speedy. Shares on the Johannesburg Inventory Change fell virtually 2 % by noon, and the rand traded at its lowest in additional than a 12 months.
South Africa itself had alerted the WHO in regards to the variant after scientists from Botswana had detected it amongst travellers who flew in from Europe. The South African overseas ministry slammed the bans. “Wonderful science must be applauded and never punished,” it mentioned.
The journey ban had knock-on results at Afrigen. Gear and chemical substances essential to creating a vaccine have been caught overseas. The airline tickets of overseas scientists who have been flying in to cooperate have been cancelled as have been these of workers due for coaching abroad. Grounded flights additionally delayed the sharing of laboratory samples of Omicron to help sooner analysis into the brand new pressure. These developments virtually totally halted international scientific collaboration and set Afrigen’s analysis again by months.

“It was an enormous drawback,” Fenner says with apparent understatement as she sits behind the desk in her small, white-walled workplace.
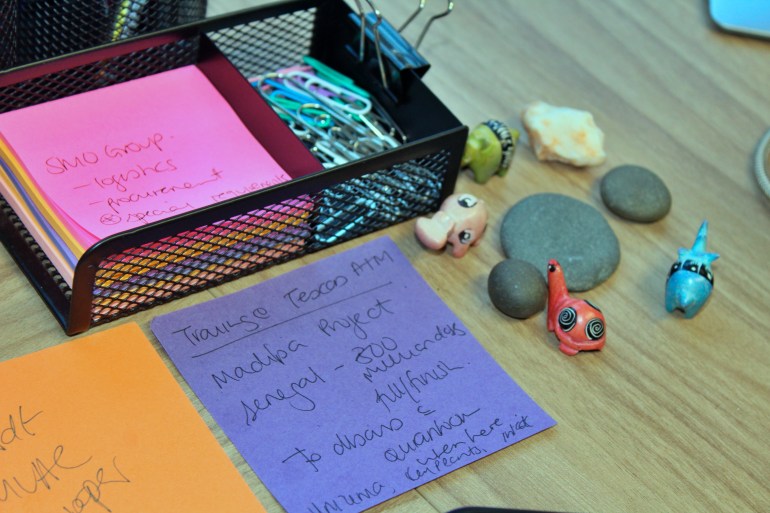
She takes a swig of water and a sombre look out of her workplace window. She is firing off emails on progress studies and shows. A handwritten observe taped to her desk reminds her of Africa’s vaccine objectives together with that Senegal goals to “fill and end” 300 million doses yearly. Week after week, Afrigen has been working across the clock to reverse-engineer Moderna’s system. For Fenner it has meant sacrificing time along with her husband and two younger youngsters.
She usually spent nights within the workplace navigating the grim realities of Africa’s logistics and procurement limitations. Then, one Wednesday night in January 2022, Fenner and her staff had a breakthrough – they'd managed to make microlitres of the vaccine – the primary copy produced virtually totally with out the help and approval of the developer.
“If we had the energetic involvement from Moderna, whether or not it might have been sooner, I don’t know, however it actually would have been simpler,” says Petro Terblanche, Afrigen’s managing director, with a steely expression behind black-rimmed spectacles.
For Terblanche, the eureka second in bringing mRNA vaccines to Africa will probably be to adapt them to an African context. mRNA molecules are wrapped inside a lipid nanoparticle due to their fragility and require excessive chilly storage. Working with Johannesburg’s College of Witwatersrand, generally referred to as Wits, the researchers plan to develop a brand new formulation for the vaccines, one which doesn’t require ultra-low freezing, which is a problem for some African international locations battling common energy outages or rural communities with none electrical energy in any respect.
“That for me might be a very powerful innovation that this hub and the scientists with Wits can do,” she provides pointedly. For now, the extra speedy hurdle is to supply extra of the reproduction vaccine, so human trials can start in Might 2023. Moderna advised Al Jazeera that the corporate is already engaged on a subsequent technology model of its shot that will be “fridge steady” for creating international locations.

Lengthy highway for African tech
Vaccines have been developed inside a 12 months of the outbreak of the COVID pandemic, however on account of a bidding battle with richer, Western nations, a lot of Africa was final in line for doses. Afrigen is the central hub of a pilot mission created by the WHO to share know-how on making mRNA vaccines with “spokes”, or producers, from greater than 20 international locations in Jap Europe, Latin America and Africa, together with Egypt, Kenya, Nigeria, Senegal and Tunisia. That call was taken after producers Moderna, Pfizer and its companion BioNTech declined to share their vaccine recipes. In South Africa, Afrigen will make the mRNA, and the Biovac Institute will manufacture the vaccines.
Whereas the demand for COVID-19 pictures will finally subside, well being specialists say way more is at stake. African international locations now import 99 % of their vaccines and 70 % of all medicines used, however the African Union has set a objective for as much as 60 % of routine immunisations to be produced on the continent by 2040.
The infrastructure to attain that purpose is proscribed. Solely 10 African producers produce vaccines towards any illness. One drawback that Afrigen needed to overcome was that, as a result of there isn’t a big pharmaceutical-driven trade in Africa, native researchers had little expertise in processing medicine to business requirements and assembly worldwide regulatory necessities.
“The scientists we will get, they're sitting in universities,” Terblanche says. “However we have to practice them to function in a vaccine facility … and never educational analysis.”
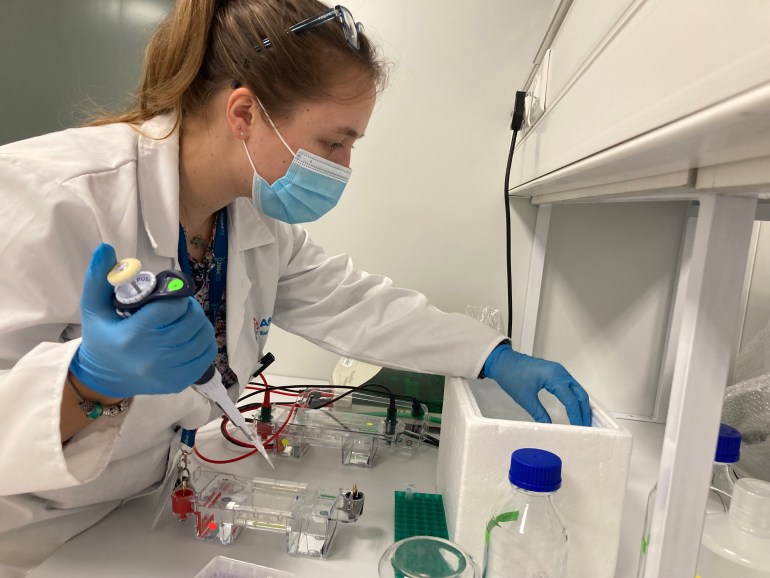
Take Frances Lees. The younger scientist joined Afrigen in January 2020 simply because the pandemic was getting underneath method. Lees had accomplished a grasp’s diploma in cell biology and had been engaged on veterinary vaccine tasks earlier than being shortly pulled into mRNA improvement as one of many few researchers who had a background in molecules.
After graduating, lots of the continent’s scientists are employed in pure scientific analysis. Producing vaccine recipes at scale is monumental work on a continent with comparatively few pharmaceutical corporations. For Lees, it required “an enormous thoughts shift”.
Talking in Afrigen’s vibrant kitchenette, which serves as a break space for employees, Lees explains that copying a producer’s vaccine with out its assist means nobody can clarify why a specific mistake occurs.
“Generally it goes mistaken, and also you don’t actually know why and it's important to repeat your experiment, so there’s quite a lot of course of that goes on that takes time,” she says. “And time isn’t our good friend in the intervening time.”
Lees believes a breakthrough would shatter a false impression that this sort of analysis and improvement can't be accomplished in Africa.
“Synthesising mRNA isn’t tremendous tough; it's making an attempt to be sure that we've got numerous it … at a high quality excessive sufficient for a vaccine,” she says. “We're not going to scrimp on uncooked supplies or make shortcuts.”
In it collectively?
Dr Hapiloe Maranyane is comparatively new at Afrigen, having began in April as a senior scientist. She stands alone within the laboratory suite, peering by security glasses and greedy a single channel pipette dropper in a single hand as she dispenses chemical substances inside a biosafety cupboard. She opens her journal to a clean web page and begins to take notes.

In business vaccine manufacturing, “it isn't simply the science that issues,” she says. “The largest problem for me was shifting from a tutorial focus to a producing focus. There may be positively a better stringency, accurately, by way of the way you document your science and high quality assurance that must be stratified and high quality management.”
When the pandemic hit, Maranyane spent six months unemployed regardless of having two doctorates in most cancers analysis and a background in infectious ailments. When she met Fenner, Afrigen’s govt director confirmed an curiosity in her background information of cell RNA and advised her that Afrigen was in search of molecular biologists and medical biochemists.
“There actually wasn’t work,” she says, recalling former colleagues – specialists within the fields of chemistry, plant and cell biology – who had deserted science to promote luggage or moved abroad to seek out jobs. “And these would have been sensible scientists, high of the category,” she says hanging a noticeably solemn observe in contrast along with her traditional boisterous giggle.
“It was trauma-inducing to undergo the pandemic and really feel powerless, not solely on a rustic degree but additionally a scientific degree,” she says.
Maranyane describes a science trade that doesn't require extremely certified workers in Africa however graduates who're in a position to repeat primary duties whereas the majority of the expert work stays the accountability of scientists primarily based out of an organization’s headquarters in Europe or the US.
“What’s distinctive about Afrigen,” she says is that “it takes a PhD mind to unravel among the questions that we face within the lab and that wouldn’t be a requirement in different environments.”

The adverse international response in the direction of the continent following the identification of Omicron cast in her thoughts why Africa must be self-sufficient.
“I felt prefer it was an unscientific response,” Maranyane says of the journey bans. “It felt as if to a point, we weren’t essentially on this collectively.” This made her extra decided to assist set up a mannequin for a way Africans can sort out future pandemics.
She arrives on the lab round 8am, her braided hair piled excessive. Her eyes alert, mumbling behind surgical masks the chemical formulation she’d memorised the evening earlier than. She is usually the final to depart the workplace.
“It was virtually set in stone that if you're desirous to do science in Africa, in South Africa, it’s a pipe dream, so I really feel very privileged to be dwelling the pipe dream now,” she says.
Doing it themselves
What is obvious in spending time at Afrigen’s lab is how a lot this highly effective crew of 20 folks, made up largely of feminine scientists, are united of their imaginative and prescient of Africa as a repository for disruptive science.
An investigation in February by the British Medical Journal revealed the kENUP Basis, a consultancy employed by BioNTech, requested the South African authorities to cease exercise by Afrigen and the WHO hub. “The sustainability outlook for this mission of the WHO Vaccine Expertise Switch Hub will not be beneficial,” kENUP mentioned in paperwork obtained by the journal. BioNTech didn't reply to Al Jazeera’s requests for remark.
As an alternative of sharing their recipes, BioNTech and Moderna plan to construct their very own vaccine crops in Africa. Critics argue these start-ups, introduced after Afrigen’s hub, are a smokescreen to keep away from sharing expertise that will eat into earnings.
In a press release, Moderna advised Al Jazeera that whereas it “has filed patents in South Africa and plenty of different international locations associated to each the COVID-19 vaccine and Moderna’s platform expertise,” the corporate is “dedicated to making sure that our mental property, or considerations about enforcement of our mental property, don't pose a barrier to entry.” Moderna’s proposed mRNA facility in Kenya has “sturdy assist from the US authorities, together with the US ambassador to Kenya, Meg Whitman,” the assertion famous.
In the meantime, Pfizer-BioNTech introduced a deal in July final 12 months with the Cape City-based Biovac Institute. It's for a bottle and pack partnership beginning this 12 months, which doesn't embody information of the vaccine’s foremost ingredient.

Pfizer pointed to the challenges in establishing native manufacturing in Africa. “Final 12 months, … water was rationed, which made it very tough each virtually but additionally ethically to acquire and use giant portions of water for trial runs by the gear as a part of our start-up,” Patrick van der Lavatory, Pfizer’s regional president for Africa and the Center East, mentioned at a convention in Rwanda. Pfizer’s spokesperson for east and southern Africa, Willis Angira, advised Al Jazeera that the corporate “has made a considerable funding within the Biovac Institute” of which the partnership “supplies vital workforce improvement coaching to healthcare professionals in South Africa”. Angira added that vaccine manufacturing “is awfully complicated underneath any circumstances, and much more so throughout a pandemic.”
Charles Gore is the chief director of the Medicines Patent Pool, a United Nations-backed non-profit that works to make medical therapy and applied sciences accessible to low- and middle-income international locations. He says African manufacturing must be about self-sufficiency. “This isn't about corporations from the developed world organising subsidiaries in Africa,” Gore says. “It's about African corporations being the recipient of tech switch to have the ability to do it themselves.”
“When it comes to vaccines, we have been advised proper initially of the pandemic basically, ‘Go away. There is no such thing as a function for you in generic manufacturing of vaccines,'” Gore says.
“There is no such thing as a query it's much more sophisticated than producing a small molecule, however sadly, pharma declined to sit down down with us and focus on whether or not the challenges might be overcome,” he says.
Reopening the AIDS dilemma
African healthcare employees say the continent has seen such resistance earlier than. Regardless of South African sufferers taking part in scientific drug trials for HIV and AIDS therapeutics, the price of the medicine that went to market was too excessive for many individuals who desperately wanted them.
In 1997, then-South African President Nelson Mandela signed into legislation an act giving the state the suitable to import and produce low cost generic variations of pricy HIV and AIDS medicine with out permission from patent holders.
This allowed the federal government to set a hard and fast worth for the medicine and the quantity of royalties paid to the patent holder, thereby lowering the price of HIV medicine by as much as 90 %.

This improvement got here after 20 years of frustration, throughout which – on account of inequity – extra folks in African international locations died after the introduction of efficient antiretrovirals than earlier than the medicine had been launched.
Practically 40 drug corporations sued South Africa in 1998. The nation was positioned on a US watchlist of countries infringing worldwide patent rights. However the corporations confronted a worldwide backlash and in 2001 withdrew their lawsuit.
Now, Afrigen and the WHO have taken on an identical problem.
In response to a 2021 report by researchers at Yale College within the US, decrease revenue nations that participated in COVID vaccine trials, together with South Africa, obtained fewer doses of the vaccines they helped take a look at than richer international locations. Excessive-income nations additionally obtained these doses forward of poorer ones.
‘A criminal offense of historic proportions’
Max Lawson, co-chairman of the Individuals’s Vaccine Alliance and head of inequality coverage at Oxfam, calls it “a criminal offense of historic proportions” that European international locations protected their pharmaceutical corporations and the vaccine provide for years.
In March, Johnson & Johnson executives agreed that a South African pharmaceutical firm, Aspen Pharmacare, would manufacture and provide doses to African international locations. By Might, Aspen was on the point of closure after receiving no orders.
Africa had moved from not having sufficient vaccines to being awash with donations “one and a half years too late”, Lawson explains. It was after a degree at which richer international locations had vaccinated greater than 80 % of their populations.
“A donation mannequin is deceptively and dangerously addictive,” Gore tells Al Jazeera. “The recipients get used to issues being given and they also count on it, which then signifies that they don’t put the sources into doing their very own improvement.”
Fatima Hassan, a human rights lawyer who heads the Well being Justice Initiative in South Africa, notes that Johnson & Johnson’s vaccine, which makes use of conventional expertise, fell out of favour globally as research discovered mRNA pictures have been simpler towards newer COVID variants.
Johnson & Johnson quickly halted manufacturing at its personal facility within the Dutch metropolis of Leiden to prioritise a doubtlessly extra worthwhile vaccine for the unrelated respiratory syncytial virus. “The purpose at which the world actually wanted the J&J vaccine was within the first quarter of final 12 months,” Hassan says.
Once I first spoke to Terblanche in January, Afrigen had aimed to fast-track scientific trials. However the firm was navigating competitors from international pharma over uncooked supplies made within the US and Europe to develop the COVID vaccines made by Moderna, Pfizer-BioNTech and Johnson & Johnson.
For 2 years, India and South Africa, backed by virtually all African nations, pushed for World Commerce Group (WTO) member international locations to waive mental property protections for COVID vaccines so manufacturing might be accomplished on the continent with out lawsuits from medicine corporations.
In response to criticism, Moderna in March pledged to “by no means implement” its patents for COVID vaccines towards producers in 92 poorer nations. South Africa was not on the record. As an alternative, Moderna registered for a broad set of patent protections within the nation.
In June, the WTO agreed on a partial patent waiver, which permits governments to compel pharmaceutical corporations to share their vaccine formulation for the subsequent 5 years – with “sufficient” compensation.
An African endgame?
Behind the scenes, a race for the subsequent technology of mRNA vaccines concentrating on quite a lot of different ailments is underneath method. Moderna and BioNTech are doing scientific trials towards influenza, HIV, dengue, Zika, hepatitis and malaria. Africa might as soon as once more be relegated to the again of the queue. That is precisely what scientists at Afrigen try to forestall.
There may be potential to rework entry to medicines for ailments affecting African international locations, Maranyane tells Al Jazeera. When there’s a brand new pandemic, African producers might manufacture their very own mRNA pictures on a big scale, Fenner says.
“Exterior of a pandemic, the concept is that these specific corporations would deal with ailments of curiosity of their area,” she says. Nigeria for instance, may select to deal with Lassa fever. It's attributable to a virus that kills 1000's of individuals within the area yearly and which epidemiologists counsel might develop into the subsequent pandemic. A number of potential vaccines are in improvement however largely by researchers inside North America.
Such makes an attempt to unravel these big challenges make scientists like Lees and Maranyane extra inclined to proceed working in Africa fairly than search alternatives abroad.

Fenner is aware of all too properly the wrestle that younger scientists face throughout Africa. Like most individuals of color in South Africa, Fenner, a fourth technology South African of Indian descent, grew up inside a combined heritage neighborhood that was impacted by racist apartheid legal guidelines.
“I all the time say after I speak about my background that I'm one of many ones that beat the chances as a result of all people didn’t have the identical combating likelihood,” she says. “My mother and father having not had all of the alternatives that have been out there didn’t even end college. They made it their precedence that every of us youngsters would end college and we’d have some type of tertiary schooling.”
Alternatives out there to scientists have been in academia however usually required researchers to safe exterior grants. For Fenner, who spent 5 years working as a tutorial researcher after incomes a doctorate in biotechnology, it grew to become “very taxing”.
Along with instructing and supervising doctoral college students, “you additionally needed to spend time having this strain of bringing in your individual wage,” she says. Because of this, she left academia and got here to work at Afrigen. “I haven’t seemed again since, and it’s been practically six years,” she says.
“We had been lobbying with the South African authorities to spend a certain quantity of the nation’s GDP on the scientific surroundings,” she provides. “The funds have been simply not there.”
A part of the push is addressing these shortfalls. As of July, there have been at the least 12 vaccine producers gearing as much as obtain Afrigen’s mRNA know-how. The equal of about $95m is required to fund Afrigen’s vaccine initiative over the subsequent 5 years. Greater than 60 % of that has been secured, Terblanche says. The cash has come from the European Fee and particular person governments, together with South Africa, France, Belgium and Canada.

Africa accounts for lower than 1 % of worldwide analysis output. For the reason that Nineteen Nineties, one in three African researchers and scientists go away the continent yearly, in accordance with UNESCO.
“You probably have cutting-edge corporations which are doing actually thrilling science, these folks will keep as a result of there are alternatives available proper on the forefront of issues in Africa,” Gore says.
Specialists within the subject say mRNA vaccines contain fewer substances and capability than conventional vaccines. Marie-Paule Kieny is the director of analysis at France’s Nationwide Institute of Well being and Medical Analysis and a WHO veteran who helped create the primary hubs in 2006 to provide poorer nations accessible flu vaccines. “It’s a expertise which may be very versatile,” Kieny says. “You don’t have to buy very costly stainless-steel gear that normally is used to supply vaccines.”
But the massive query is whether or not African governments can preserve the political and monetary dedication wanted over time. “Even when we're in a position to manufacture all these vaccines, the place do they go?” Fenner asks. “In order that’s the larger dialog. Do the governments that we're in and the particular international locations the place the spokes [manufacturers] are primarily based, are they then going to incentivise the native manufacturing and say, ‘Sure, we are going to buy vaccines from you’?”
African public well being officers ought to prioritise vaccine manufacturing as a nationwide technique as a result of, crucially, vaccine builders are within the enterprise to make a revenue and can prioritise markets the place their sponsors are primarily based, says Bartholomew Dicky Akanmori, the regional adviser for vaccine analysis and regulation for WHO throughout Africa.
“COVID-19 taught us that inequity does exist in entry to well being and that in relation to a scenario such because the pandemic, international locations would rightfully think about their populations first,” he notes. “But when African governments begin investing in their very own analysis and improvement, in the end, they'll personal the mental property.”

Post a Comment